Search
- Page Path
- HOME > Search
- Thyroid
- Corrigendum: Abstract and Text Correction. Thyroid Stimulating Hormone Reference Range and Prevalence of Thyroid Dysfunction in the Korean Population: Korea National Health and Nutrition Examination Survey 2013 to 2015
- Won Gu Kim, Won Bae Kim, Gyeongji Woo, Hyejin Kim, Yumi Cho, Tae Yong Kim, Sun Wook Kim, Myung-Hee Shin, Jin Woo Park, Hai-Lin Park, Kyungwon Oh, Jae Hoon Chung
- Endocrinol Metab. 2023;38(3):357. Published online May 16, 2023
- DOI: https://doi.org/10.3803/EnM.2023.301
- Corrects: Endocrinol Metab 2017;32(1):106
- 1,285 View
- 62 Download

- Thyroid
- Identification of Mutations in the Thyroxine-Binding Globulin (TBG) Gene in Patients with TBG Deficiency in Korea
- Jung Heo, Sang-Mi Kim, Hyun Jin Ryu, Hyunju Park, Tae Hyuk Kim, Jae Hoon Chung, Hyung-Doo Park, Sun Wook Kim
- Endocrinol Metab. 2022;37(6):870-878. Published online December 7, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1591
- 1,750 View
- 198 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
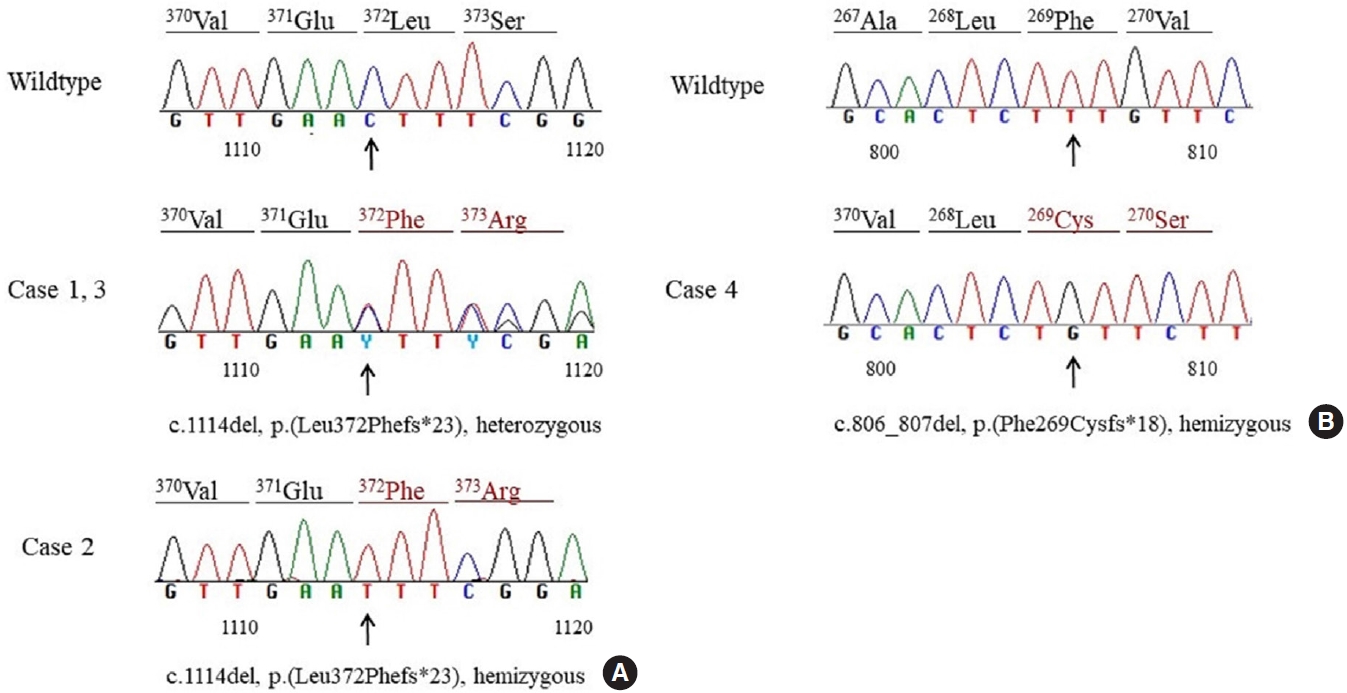
Thyroxine-binding globulin (TBG) is a major transporter protein for thyroid hormones. The serpin family A member 7 (SERPINA7) gene codes for TBG, and mutations of the SERPINA7 gene result in TBG deficiency. Although more than 40 mutations have been reported in several countries, only a few studies of TBG deficiency and SERPINA7 gene mutation have been performed in Korea. The aim of this study is to review the clinical presentations and laboratory findings of patients with TBG deficiency and to investigate the types of SERPINA7 gene mutation.
Methods
Five unrelated Korean adults with TBG deficiency attending endocrinology clinic underwent SERPINA7 gene sequencing. Four patients harbored a SERPINA7 gene mutation. Serum thyroid hormones, anti-microsomal antibodies, and TBG were measured. Genomic DNA was extracted from whole blood. All exons and intron-exon boundaries of the TBG gene were amplified and sequencing was performed.
Results
Two patients were heterozygous females, and the other two were hemizygous males. One heterozygous female had coexisting hypothyroidism. The other heterozygous female was erroneously prescribed levothyroxine at a local clinic. One hemizygous male harbored a novel mutation, p.Phe269Cysfs*18, which caused TBG partial deficiency. Three patients had the p.Leu372Phefs*23 mutation, which is known as TBG-complete deficiency Japan (TBG-CDJ) and was also presented in previous mutation analyses in Korea.
Conclusion
This study presents four patients diagnosed with TBG deficiency and provides the results of SERPINA7 gene sequencing. One novel mutation, p.Phe269Cysfs*18, causing TBD-partial deficiency and three cases of TBG-CDJ were demonstrated. It is necessary to identify TBG deficiency to prevent improper treatment. Also, sequencing of the SERPINA7 gene would provide valuable information about the TBG variants in Korea. -
Citations
Citations to this article as recorded by- Development and basic performance verification of a rapid homogeneous bioassay for agonistic antibodies against the thyroid-stimulating hormone receptor
Motoki Hoshina, Shiomi Ojima, Atsushi Kawasaki, Kosuke Doi, Satoshi Ohta, Asuka Inoue, Hiroshi Murayama
Journal of Immunological Methods.2024; 528: 113655. CrossRef
- Development and basic performance verification of a rapid homogeneous bioassay for agonistic antibodies against the thyroid-stimulating hormone receptor

- Thyroid
- Frequency of TERT Promoter Mutations in Real-World Analysis of 2,092 Thyroid Carcinoma Patients (Endocrinol Metab 2022;37:652-63, Heera Yang et al.)
- Hyunju Park, Jae Hoon Chung
- Endocrinol Metab. 2022;37(6):949-950. Published online November 10, 2022
- DOI: https://doi.org/10.3803/EnM.2022.601
- [Original]
- 1,380 View
- 152 Download

- Thyroid
- Frequency of TERT Promoter Mutations in Real-World Analysis of 2,092 Thyroid Carcinoma Patients
- Heera Yang, Hyunju Park, Hyun Jin Ryu, Jung Heo, Jung-Sun Kim, Young Lyun Oh, Jun-Ho Choe, Jung Han Kim, Jee Soo Kim, Hye Won Jang, Tae Hyuk Kim, Sun Wook Kim, Jae Hoon Chung
- Endocrinol Metab. 2022;37(4):652-663. Published online July 22, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1477
- 3,626 View
- 193 Download
- 11 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
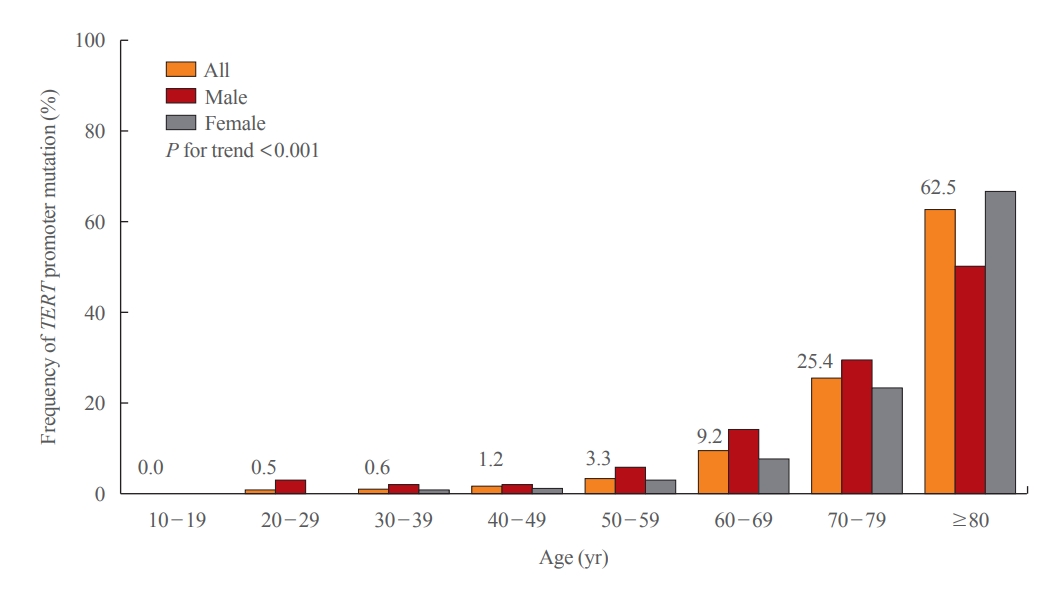
Telomerase reverse transcriptase (TERT) promoter mutations are associated with increased recurrence and mortality in patients with thyroid carcinoma. Previous studies on TERT promoter mutations were retrospectively conducted on a limited number of patients.
Methods
We prospectively collected data on all consecutive patients who underwent thyroid carcinoma surgery between January 2019 and December 2020 at the Samsung Medical Center, Seoul, Korea. We included 2,092 patients with thyroid carcinoma.
Results
Of 2,092 patients, 72 patients (3.4%) had TERT promoter mutations. However, the frequency of TERT promoter mutations was 0.5% in papillary thyroid microcarcinoma (PTMC) ≤1 cm and it was 5.8% in papillary thyroid carcinoma (PTC) >1 cm. The frequency of TERT promoter mutations was significantly associated with older age at diagnosis (odds ratio [OR], 1.12; P<0.001), larger primary tumor size (OR, 2.02; P<0.001), and aggressive histological type (OR, 7.78 in follicular thyroid carcinoma; OR, 10.33 in poorly differentiated thyroid carcinoma; OR, 45.92 in anaplastic thyroid carcinoma; P<0.001). Advanced T stage, advanced N stage, and distant metastasis at diagnosis were highly prevalent in mutated thyroid cancers. However, initial distant metastasis was not present in patients with TERT promoter mutations in PTMC. Although the C228T mutation was more highly detected than the C250T mutation (64 cases vs. 7 cases), there were no significant clinicopathological differences.
Conclusion
This study is the first attempt to investigate the frequency of TERT promoter mutations in a real-world setting. The frequency of TERT promoter mutations in PTC was lower than expected, and in PTMC, young patients, and female patients, the frequency was very low. -
Citations
Citations to this article as recorded by-
TERT Promoter Mutations Frequency Across Race, Sex, and Cancer Type
Talal El Zarif, Marc Machaalani, Rashad Nawfal, Amin H Nassar, Wanling Xie, Toni K Choueiri, Mark Pomerantz
The Oncologist.2024; 29(1): 8. CrossRef - Gene mutations as predictors of central lymph mode metastasis in cN0 PTC: A meta‐analysis
Jiaqi Ji, Xinlong Shi
Clinical Genetics.2024; 105(2): 130. CrossRef - Risk stratification by combining common genetic mutations and TERT promoter methylation in papillary thyroid cancer
Ye Sang, Guanghui Hu, Junyu Xue, Mengke Chen, Shubin Hong, Rengyun Liu
Endocrine.2024;[Epub] CrossRef - Shortened telomere length in peripheral blood leukocytes is associated with cumulative radioactive iodine doses in patients with differentiated thyroid carcinoma
Hoonsung Choi, Sun Wook Cho, Hwan Hee Kim, Ka Hee Yi, Do Joon Park, Young Joo Park
Cancer.2024;[Epub] CrossRef - Deciphering the Functions of Telomerase Reverse Transcriptase in Head and Neck Cancer
Tsung-Jang Yeh, Chi-Wen Luo, Jeng-Shiun Du, Chien-Tzu Huang, Min-Hung Wang, Tzer-Ming Chuang, Yuh-Ching Gau, Shih-Feng Cho, Yi-Chang Liu, Hui-Hua Hsiao, Li-Tzong Chen, Mei-Ren Pan, Hui-Ching Wang, Sin-Hua Moi
Biomedicines.2023; 11(3): 691. CrossRef - 2023 Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules
Young Joo Park, Eun Kyung Lee, Young Shin Song, Soo Hwan Kang, Bon Seok Koo, Sun Wook Kim, Dong Gyu Na, Seung-Kuk Baek, So Won Oh, Min Kyoung Lee, Sang-Woo Lee, Young Ah Lee, Yong Sang Lee, Ji Ye Lee, Dong-Jun Lim, Leehi Joo, Yuh-Seog Jung, Chan Kwon Jung
International Journal of Thyroidology.2023; 16(1): 1. CrossRef - Thyroid Cancer, Iodine, and Gene Mutation
Jae Hoon Chung
International Journal of Thyroidology.2023; 16(1): 89. CrossRef - Mortality rate and causes of death in papillary thyroid microcarcinoma
Jung Heo, Hyun Jin Ryu, Hyunju Park, Tae Hyuk Kim, Sun Wook Kim, Young Lyun Oh, Jae Hoon Chung
Endocrine.2023; 83(3): 671. CrossRef - TERT promoter mutations in thyroid cancer
Michiko Matsuse, Norisato Mitsutake
Endocrine Journal.2023; 70(11): 1035. CrossRef - TERT Promoter and BRAF V600E Mutations in Papillary Thyroid Cancer: A Single-Institution Experience in Korea
Min Jhi Kim, Jin Kyong Kim, Gi Jeong Kim, Sang-Wook Kang, Jandee Lee, Jong Ju Jeong, Woong Youn Chung, Daham Kim, Kee-Hyun Nam
Cancers.2022; 14(19): 4928. CrossRef - Frequency of TERT Promoter Mutations in Real-World Analysis of 2,092 Thyroid Carcinoma Patients (Endocrinol Metab 2022;37:652-63, Heera Yang et al.)
Hyunju Park, Jae Hoon Chung
Endocrinology and Metabolism.2022; 37(6): 949. CrossRef - Frequency of TERT Promoter Mutations in Real-World Analysis of 2,092 Thyroid Carcinoma Patients (Endocrinol Metab 2022;37:652-63, Heera Yang et al.)
Sue Youn Kim, Chan Kwon Jung
Endocrinology and Metabolism.2022; 37(6): 947. CrossRef
-
TERT Promoter Mutations Frequency Across Race, Sex, and Cancer Type

- Calcium & Bone Metabolism
- Bone Mineral Density Screening Interval and Transition to Osteoporosis in Asian Women
- Hyunju Park, Heera Yang, Jung Heo, Hye Won Jang, Jae Hoon Chung, Tae Hyuk Kim, Yong-Ki Min, Sun Wook Kim
- Endocrinol Metab. 2022;37(3):506-512. Published online June 9, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1429

- 3,054 View
- 103 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Bone mineral density (BMD) testing is indicated for women aged 65 years, but screening strategies for osteoporosis are controversial. Currently, there is no study focusing on the BMD testing interval in Asian populations. The current study aimed to evaluate the estimated time interval for screening osteoporosis.
Methods
We conducted a study of 6,385 subjects aged 50 years and older who underwent dual-energy X-ray absorptiometry screening more than twice at Samsung Medical Center as participants in a routine health checkup. Subjects were divided based on baseline T-score into mild osteopenia (T-score, <–1.0 to >–1.5), moderate osteopenia (T-score, ≤–1.5 to >–2.0), and severe osteopenia (T-score, ≤–2.0 to >–2.5). Information about personal medical and social history was collected by a structured questionnaire.
Results
The adjusted estimated BMD testing interval for 10% of the subjects to develop osteoporosis was 13.2 years in mild osteopenia, 5.0 years in moderate osteopenia, and 1.5 years in severe osteopenia.
Conclusion
Our study provides extended information about BMD screening intervals in Asian female population. Baseline T-score was important for predicting BMD screening interval, and repeat BMD testing within 5 years might not be necessary in mild osteopenia subjects. -
Citations
Citations to this article as recorded by- Effects of Bazedoxifene/Vitamin D Combination Therapy on Serum Vitamin D Levels and Bone Turnover Markers in Postmenopausal Women with Osteopenia: A Randomized Controlled Trial
Chaiho Jeong, Jeonghoon Ha, Jun-Il Yoo, Young-Kyun Lee, Jung Hee Kim, Yong-Chan Ha, Yong-Ki Min, Dong-Won Byun, Ki-Hyun Baek, Ho Yeon Chung
Journal of Bone Metabolism.2023; 30(2): 189. CrossRef - Bone-modifying agents for non–small-cell lung cancer patients with bone metastases during the era of immune checkpoint inhibitors: A narrative review
Jinyoung Kim, Chaiho Jeong, Jeongmin Lee, Jeonghoon Ha, Ki-Hyun Baek, Seohyun Kim, Tai Joon An, Chan Kwon Park, Hyoung Kyu Yoon, Jeong Uk Lim
Seminars in Oncology.2023; 50(3-5): 105. CrossRef
- Effects of Bazedoxifene/Vitamin D Combination Therapy on Serum Vitamin D Levels and Bone Turnover Markers in Postmenopausal Women with Osteopenia: A Randomized Controlled Trial

- Thyroid
Big Data Articles (National Health Insurance Service Database) - Graves’ Disease and the Risk of End-Stage Renal Disease: A Korean Population-Based Study
- Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Hye Ryoun Jang, Bo-Yeon Kim, Chan-Hee Jung, Jae Hyeon Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
- Endocrinol Metab. 2022;37(2):281-289. Published online April 6, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1333
- 3,895 View
- 134 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Hyperthyroidism is associated with an increased glomerular filtration rate (GFR) in the hyperdynamic state, which is reversible after restoring euthyroidism. However, long-term follow-up of renal dysfunction in patients with hyperthyroidism has not been performed.
Methods
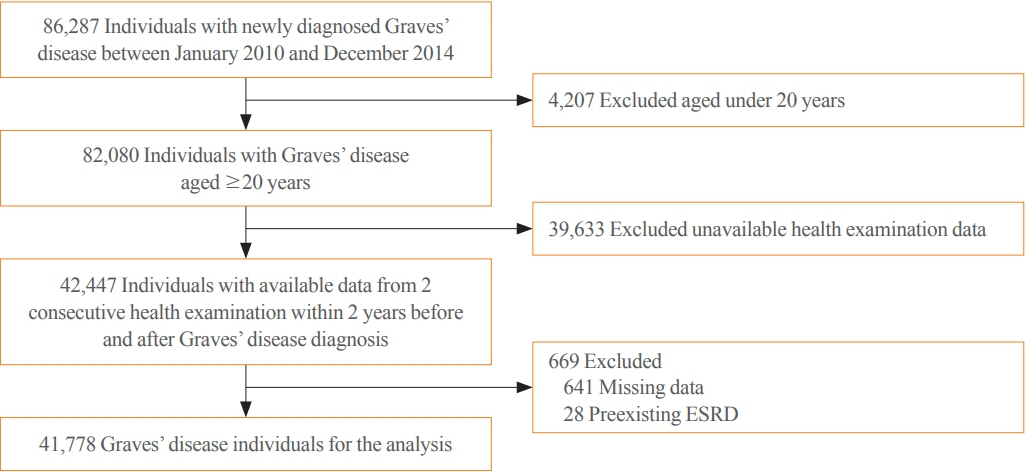
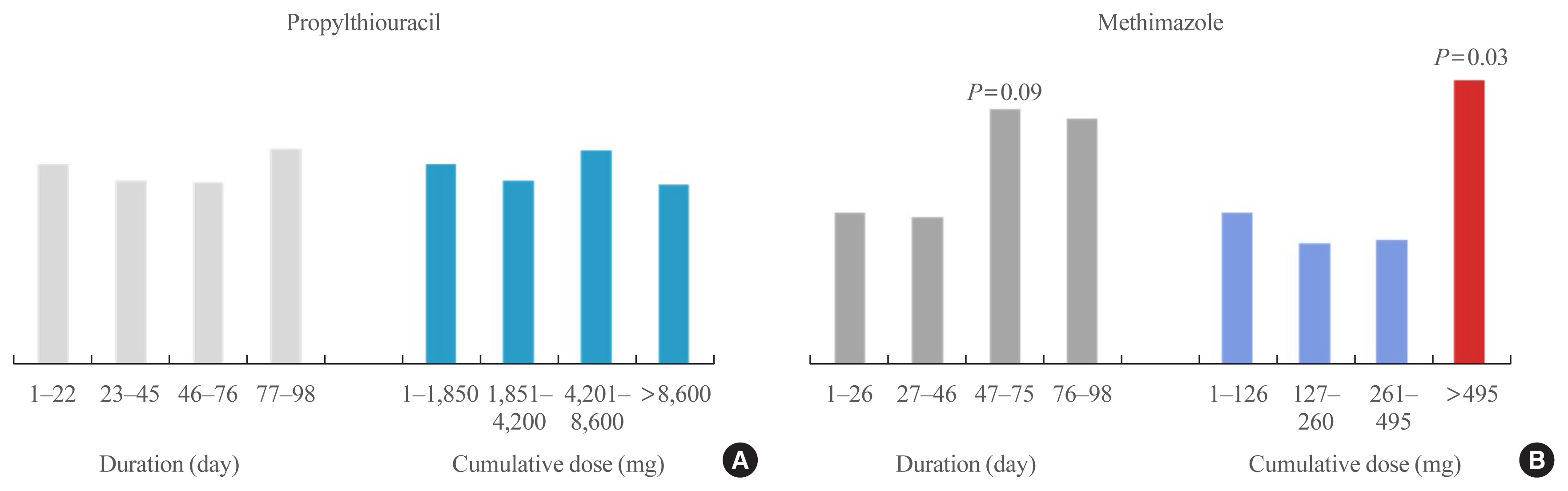
This was a retrospective cohort study using the Korean National Health Insurance database and biannual health checkup data. We included 41,778 Graves’ disease (GD) patients and 41,778 healthy controls, matched by age and sex. The incidences of end-stage renal disease (ESRD) were calculated in GD patients and controls. The cumulative dose and duration of antithyroid drugs (ATDs) were calculated for each patient and categorized into the highest, middle, and lowest tertiles.
Results
Among 41,778 GD patients, 55 ESRD cases occurred during 268,552 person-years of follow-up. Relative to the controls, regardless of smoking, drinking, or comorbidities, including chronic kidney disease, GD patients had a 47% lower risk of developing ESRD (hazard ratio [HR], 0.53; 95% confidence interval [CI], 0.37 to 0.76). In particular, GD patients with a higher baseline GFR (≥90 mL/min/1.73 m2; HR, 0.33; 95% CI, 0.11 to 0.99), longer treatment duration (>33 months; HR, 0.31; 95% CI, 0.17 to 0.58) or higher cumulative dose (>16,463 mg; HR, 0.29; 95% CI, 0.15 to 0.57) of ATDs had a significantly reduced risk of ESRD.
Conclusion
This was the first epidemiological study on the effect of GD on ESRD, and we demonstrated that GD population had a reduced risk for developing ESRD. -
Citations
Citations to this article as recorded by- Renal function changes in patients with subclinical hyperthyroidism: a novel postulated mechanism
Magdy Mohamed Allam, Hanaa Tarek El-Zawawy, Tarek Hussein El-Zawawy
Endocrine.2023; 82(1): 78. CrossRef - Effect of Hyperthyroidism on Preventing Renal Insufficiency
Tae Yong Kim
Endocrinology and Metabolism.2022; 37(2): 220. CrossRef - Effects and Clinical Value of Peritoneal Dialysis on Water and Water Balance, Adverse Reactions, Quality of Life, and Clinical Prognosis in Patients with Decompensated Chronic Nephropathy: A Systematic Review and Meta-Analysis
Xichao Wang, Miaomiao Zhang, Na Sun, Wenxiu Chang, Gang Chen
Computational and Mathematical Methods in Medicine.2022; 2022: 1. CrossRef
- Renal function changes in patients with subclinical hyperthyroidism: a novel postulated mechanism

- Thyroid
- Antithyroid Drug Treatment in Graves’ Disease
- Jae Hoon Chung
- Endocrinol Metab. 2021;36(3):491-499. Published online June 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1070
- 4,988 View
- 338 Download
- 6 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Graves’ disease is associated with thyrotropin (TSH) receptor stimulating antibody, for which there is no therapeutic agent. This disease is currently treated through inhibition of thyroid hormone synthesis or destruction of the thyroid gland. Recurrence after antithyroid drug (ATD) treatment is common. Recent studies have shown that the longer is the duration of use of ATD, the higher is the remission rate. Considering the relationship between clinical outcomes and iodine intake, recurrence of Graves’ disease is more common in iodine-deficient areas than in iodine-sufficient areas. Iodine restriction in an iodine-excessive area does not improve the effectiveness of ATD or increase remission rates. Recently, Danish and Korean nationwide studies noted significantly higher prevalence of birth defects in newborns exposed to ATD during the first trimester compared to that of those who did not have such exposure. The prevalence of birth defects was lowest when propylthiouracil (PTU) was used and decreased by only 0.15% when methimazole was changed to PTU in the first trimester. Therefore, it is best not to use ATD in the first trimester or to change to PTU before pregnancy.
-
Citations
Citations to this article as recorded by- Выраженность окислительного стресса и энзиматическая активность нейтрофилов крови у пациентов с болезнью Грейвса в зависимости от компенсации гипертиреоза
М. А. Дудина, С. А. Догадин, А. А. Савченко, И. И. Гвоздев
Ateroscleroz.2023; 18(4): 411. CrossRef - Application of oral inorganic iodine in the treatment of Graves’ disease
Yixuan Huang, Yihang Xu, Murong Xu, Xiaotong Zhao, Mingwei Chen
Frontiers in Endocrinology.2023;[Epub] CrossRef - Sex-specific risk factors associated with graves’ orbitopathy in Korean patients with newly diagnosed graves’ disease
Jooyoung Lee, Jinmo Kang, Hwa Young Ahn, Jeong Kyu Lee
Eye.2023; 37(16): 3382. CrossRef - Methimazole, an Effective Neutralizing Agent of the Sulfur Mustard Derivative 2-Chloroethyl Ethyl Sulfide
Albert Armoo, Tanner Diemer, Abigail Donkor, Jerrod Fedorchik, Severine Van slambrouck, Rachel Willand-Charnley, Brian A. Logue
ACS Bio & Med Chem Au.2023; 3(5): 448. CrossRef - Increased risk of incident gout in patients with hyperthyroidism: a nationwide retrospective cohort study
Ju-Yeun Lee, So-Yeon Park, Seo Young Sohn
Rheumatology International.2023; 44(3): 451. CrossRef - The influence of thionamides on intra-thyroidal uptake of 131I during radioiodine-131 treatment of Graves’ disease
Christian Happel, Benjamin Bockisch, Britta Leonhäuser, Amir Sabet, Frank Grünwald, Daniel Groener
Scientific Reports.2023;[Epub] CrossRef - Usefulness of Real-Time Quantitative Microvascular Ultrasonography for Differentiation of Graves’ Disease from Destructive Thyroiditis in Thyrotoxic Patients
Han-Sang Baek, Ji-Yeon Park, Chai-Ho Jeong, Jeonghoon Ha, Moo Il Kang, Dong-Jun Lim
Endocrinology and Metabolism.2022; 37(2): 323. CrossRef - The chemiluminescent and enzymatic activity of blood neutrophils in patients with Graves' disease depending on hyperthyroidism compensation
M. A. Dudina, A. A. Savchenko, S. A. Dogadin, I. I. Gvozdev
Clinical and experimental thyroidology.2022; 18(1): 4. CrossRef - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
Endocrinology and Metabolism.2021; 36(6): 1277. CrossRef
- Выраженность окислительного стресса и энзиматическая активность нейтрофилов крови у пациентов с болезнью Грейвса в зависимости от компенсации гипертиреоза

- Thyroid
- Update on Thyroid Hormone Levels and Thyroid Dysfunction in the Korean Population Based on Data from the Korea National Health and Nutrition Examination Survey VI (2013 to 2015)
- Jae Hoon Chung
- Endocrinol Metab. 2020;35(1):7-13. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.7
- 6,960 View
- 150 Download
- 7 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
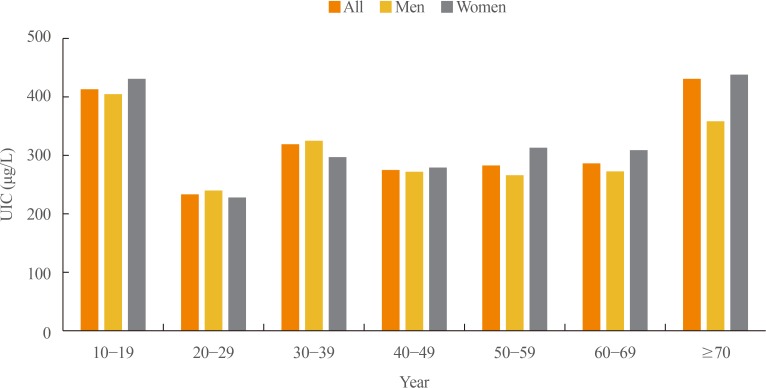
ePub In 2017, the first Korean nationwide data on serum thyroid stimulating hormone (TSH) levels, serum free thyroxine (fT4) levels, and urinary iodine concentration (UIC) were published based on a population of 7,061 Koreans who participated in the Korea National Health and Nutrition Examination Survey VI. The mean TSH level was 2.16 mIU/L, with a reference interval of 0.59 to 7.03 mIU/L (men 2.09 mIU/L, women 2.24 mIU/L,
P <0.001). A U-shaped association was found between serum TSH levels and age. The mean fT4 level was 1.25 ng/dL, and its reference interval was 0.92 to 1.60 ng/dL (men 1.29 ng/dL, women 1.20 ng/dL,P <0.0001). Serum fT4 levels decreased with age (P for trend <0.0001). Serum thyroid peroxidase antibody (TPOAb) was detected in 7.30% of participants (men 4.33%, women 10.62%). TPOAb titers tended to increase with age, and were higher in women than in men. The median UIC was 294 µg/L, and UIC showed a U-shaped relationship with age. According to the World Health Organization recommendations, only 23% of participants were in the adequate range of iodine intake, while 65% were in the above requirements or excessive, and 12% in insufficient. The prevalence of overt hyperthyroidism and hypothyroidism in Koreans was 0.34% to 0.54% and 0.73% to 1.43%, respectively.-
Citations
Citations to this article as recorded by- Association between Thyroid Function and Insulin Resistance Indices in Korean Adolescents: Findings from the 2014–2015 Korea National Health and Nutrition Examination Survey
Eunji Mun, Hye Ah Lee, Jung Eun Choi, Rosie Lee, Kyung Hee Kim, Hyesook Park, Hae Soon Kim
Children.2024; 11(3): 370. CrossRef - Diagnostic Value of Carotid Plaque Assessment with AIS Based on Quantitative Parameters of Dual-Layer Detector Spectral CT
Xiaoying Meng, Fei Li, Wenpei Wu, Juncang Wu
International Journal of General Medicine.2024; Volume 17: 1263. CrossRef - Hyperthyroidism
Sun Y. Lee, Elizabeth N. Pearce
JAMA.2023; 330(15): 1472. CrossRef - Exploring the Association between Thyroid Function and Frailty: Insights from Representative Korean Data
Youn-Ju Lee, Min-Hee Kim, Dong-Jun Lim, Jung-Min Lee, Sang Ah Chang, Jeongmin Lee
Endocrinology and Metabolism.2023; 38(6): 729. CrossRef - Subclinical Hypothyroidism: Prevalence, Health Impact, and Treatment Landscape
Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2021; 36(3): 500. CrossRef - Association between Iodine Intake, Thyroid Function, and Papillary Thyroid Cancer: A Case-Control Study
Kyungsik Kim, Sun Wook Cho, Young Joo Park, Kyu Eun Lee, Dong-Wook Lee, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 790. CrossRef
- Association between Thyroid Function and Insulin Resistance Indices in Korean Adolescents: Findings from the 2014–2015 Korea National Health and Nutrition Examination Survey

- A Case of Diabetes Insipidus with Langerhans Cell Histiocytosis in Adult.
- Jae Hoon Chung, Kwang Won Kim, Kyu Jeung Ahn, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee, Eun Mi Koh, Choon Kwan Kim, Mann Pyo Jung
- J Korean Endocr Soc. 1996;11(3):330-335. Published online November 7, 2019
- 1,199 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - In Langerhans cell histiocytosis, diabetes insipidus is the most common endocrinologic complication. We experienced a case of Langerhans cell histiocytosis, involving pituitary stalk and lung. The patient was a 43 year old male with complaint of polyuria and polydipsia. The water deprivation test was carried out to confirm the diagnosis of diabetes insipidus. We found multiple small cysts and nodules in HRCT of lung, and diagnosed Langerhans cell histiocytosis by transbronchial lung biopsy, The patient was managed conservatively with DDAVP nasal spray. The polyuria,polydipsia was relieved completely. After that, we follow up and observe closely the patients lung and pituitary lesion.

- Two cases of 111Indium Pentetreotide Scan for the Pre- and Post-Operative Evaluation of Localization and Metastasis in Medullary Thyroid Carcinoma.
- Jae Hoon Chung, Kwang Won Kim, Kyu Jeung Ahn, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee, Kyoung Ah Kim, Yeun Sun Kim, Eun Mi Koh
- J Korean Endocr Soc. 1996;11(1):85-92. Published online November 7, 2019
- 1,054 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - Medullary carcinoma of the thyroid gland(MTC) constitutes approximatesly 3% to 10% of all malignant thyroid tumors. It appears in both familial and sporadic forms. Metastases are frequently present at diagnosis and are resistant to chemotherapy and radiotherapy. Surgical resection of the primary tumor and the metastases is the mainstay of treatment. Although MTC can be detected by elevated serum calcitonin, localization of residual or metastatic foci may be difficult. Many scintigraphic methods have been used for identification of the residual tumor or metastasis. However, most of them have either low sensitivity or low specificity. MTC frequently secretes somatostatin and may express somatostatin receptors. Recently, somatostatin-receptor imaging has been known to be useful for the detection of residual and recurrent medullary thyroid carcinoma. A 25 year-old woman who was dignosed as medullary carcinoma by biopsy of thyroid mass is presented. Thirteen years ago, she underwent left thyroidectomy due to thyroid cancer(MTC). Laboratory tests revealed an increase in the levels in serum CEA(CEA=557.6 ng/ml) and calcitonin(calcitonin= 720 pg/ml). The second patient, a 30 year-old female, complained of a palpable mass in the left anterior neck. Ten years ago, she underwent a right lobectomy of thyroid gland due to adenomatous goiter. Laboratory tests revealed an increase in the levels in serum CEA(CEA=617 ng/ml) and Calcitonin (Calcitonin=2,300 pg/ml). In both cases, pre- and postoperative In-111 pentetreotide scintigraphy were done and compared with "'I scintigraphy. In-111 pentetreotide scan may be useful for the localization of residual or metastatic medullary thyroid carcinoma. Further study is warranted to define the sensitivity and specificity of the technique.

- Spontaneous Recovery from Hypothyroidism in Autommune Thyroiditis.
- Bo Youn Cho, Jae Hoon Chung, Kwang Won Kim, Kyu Jeung Ahn, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee
- J Korean Endocr Soc. 1996;11(1):30-40. Published online November 7, 2019
- 2,191 View
- 34 Download
-
 Abstract
Abstract
 PDF
PDF - Background
A lifelong thyroxine therapy is indicated in all patients who have hypothyroidism as a result of autoimmune thyroiditis. However, it has been reported that some hypothyroid patients with autoimmune thyroiditis have spontaneous remission with restriction of iodine intake instead of thyroxine therapy. The purpose of study was to investigate how many hypothyroid patients with autoimmune thyroiditis can recover from hypothyroidism with restriction of iodine intake instead of thyroxine therapy and which factors predict recovery from hypothyroidism. Methods: We studied 64 patients with autoimmune thyroiditis(goitrous autoimmune thyroiditis 56, atrophic autoimmune thyroiditis 8). Thyroxine therapy was discontinued in patients with goitrous autoimmune thyroiditis on the way(group 1, n=32) or from the beginning(group 2, n=24) and atrophic autoimmune thyroiditis on the way(group 3, n-8). All patients were asked to avoid iodine-rich foods and thyroid function was monitored every one to two months for up to 35 months. Serum T3, T4, TSH concentrations, antithyroglobulin and antimicrosomal antibodies were measured by radioimmunoassay(RIA). TSH binding inhibitor immunoglobulin(TBII) was measured in serum using radioreceptor assay. Two hundred micrograms of thyrotropin releasing hormone (TRH) were given as intravenous bolus and TSH levels were measured in blood samples taken at 0, 30, and 60 minutes. All values were expressed as mean+-SEM. Statistical analysis was done with paired or non-paired t-test, ANOVA, and the Chi-square test. Statistical significance was defined as p-value below 0.05. Results: Thirteen(40.6%) of 32 patients in group 1 remained euthyroid after 12-35 months of discontinuation of thyroxine therapy. The other 19(59.4%) patients in group 1 had recurrences of hypothyroidism within 3 months after discontinuation of thyroxine therapy. In 11(45.8%) out of 24 patients in group 2, serum TSH concentrations declined below 5 mU/L within 3 months without thyroxine therapy. The other 13(54.2%) patients in group 2 remained hypothyroid till 2-16 months and the thyroxine was given. In contrast, all 8 patients in group 3 had recurrences of hypothy- roidism within 3 months after stopping thyroxine therapy. When we compared the recovered patients of goitrous autoimmune thyroiditis with the non-recovered patients of goitrous autoimmune thyroiditis, regardless of thyroxine therapy from the beginning, age at onset of disease of the 24 recovered patients was significantly younger than the 32 non-recovered patients(30.1+2.0 years vs. 40.2+ 2.4 years; p=0.004). Concl#usion: These findings suggest that 42.9% of hypothyroid patients with goitrous autoim- mune thyroiditis remain or become spontaneously euthyroid with restriction of iodine intake instead of thyroxine therapy. Young age may be a predicting factor of recovery from hypothyroidism in goitrous autoimmune thyroiditis.

- Assay of Thyrotropin Receptor Antibodies with Recombinant Human Thyrotropin Receptor Expressed on Chinese Hamster Ovary Cells.
- Bo Youn Cho, Hong Kyu Lee, Chang Soon Koh, Jae Hoon Chung, Ka Hee Yi, Kyung Soo Ko, Won Bae Kim
- J Korean Endocr Soc. 1995;10(4):347-361. Published online November 7, 2019
- 1,168 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Thyroid stimulating antibody which results in the development of hyperthyroidism and goiter in Graves' patients used to be measured by using rat thyroid cells, FRTL-5. However, this assay has disadvantages: decreased sensitivity due to differences in species, and fastidious culture conditions for FRTL-5 cells. Thus, we recently created stably transfected Chinese hamster ovary(CHO) cells containing the human TSH receptor(hTSHR-CHO) and developed optimal conditions for the measurement of thyroid stimulating antibody using hTSHR-CHO cells. In this study, to evaluate the clinical relevance of thyroid stimulating antibody measurement using hTSHR-CHO cells, we measured thyroid stimulating antibody activities of IgGs from Graves' disease and other thyroid disease using hTSHR-CHO cells, and compared to those of thyroid stimulating antibody assays using FRTL-5 cells. 1) The cut off value of positive thyroid stimulating antibody activity measured in hTSHR-CHO cells was 145%(above the mean +2SD) which was lower than 165% in FRTL-5 cells. The intra-assay and inter-assay variances were 3.9% to 9.0% and 12.7% to 1.6%, respectively. 2) Thyroid stimulating antibody activity was detected in 90% of patients with untreated Graves' disease when patients initially presented. Further, in patients seen initially but already under therapy, 75% had positive values if they were hyperthyroid but only 43% had IgGs with activity if they were euthyroid. Patients in clinical remission after therapy showed positive values in 23% of cases. Only 2 of 25 patients with Hashimoto's thyroiditis showed weak thyroid stimulating antibody activity, none of 18 patients with nodular nontoxie goiter, 1 of 15 patients with primary myxedema, and 2 of 33 control patients with no thyroid disease. Thus, the detection frequency and specificity of the assay with hTSHR-CHO cells was excellent for this type bioassay.3) The detection frequency of thyroid stimulating antibody activity by hTSHR-CHO cells assay system(90%) was higher than that by FRTL-5 cells assay system(66%) in untreated Graves' patients. Those two activities were positively correlated with each other(r=0.52, p<0.001). However, some IgGs showed discrepancy of the thyroid stimulating antibody activity measured in hTSHR-CHO cells and in FRTL-5 cells; 56 of 87 patients were positive in both cells system, 8 of 87 were negative in both cells system, 1 of 87 was only positive in FRTL-5 cells and 22 of 87 were only positive in hTSHR-CHO cell system. Thus, 73%(22/30) of IgGs showing negative values of thyroid stimulating antibody activities in FRTL-5 cells were detected its activities in hTSHR-CHO cells system.In summary, thyroid stimulating antibody assay with hTSHR-CHO cells exhibited so excellent sensitivity and specificity that this technique should be used for clinical practice as well as basic research.

- Changes in Thyrotropin Receptor Blocking Antibody after Antithyroid drug Administration to Patients with Atrophic Autoimmune Thyroiditis (Primary Myxedema).
- Seong Yeon Kim, Bo Youn Cho, Hong Kyu Lee, Jae Hoon Chung, Chang Soon Koh, Chan Soo Shin, Won Bae Kim
- J Korean Endocr Soc. 1994;10(3):229-241. Published online November 6, 2019
- 1,066 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - It is well Known that antithyroid drug treatment of Graves' disease suppresses excessive thyroid hormone synthesis and causes a parallel decrease in serum thyroid autoantibody levels including thyroid stimulating antibodies(TSAb) in most patients suggesting the immunosuppressive or immunomodulating effects of antithyroid drugs. In the context of view that thyrotropin receptor blocking antibody may play an important pathogenetic role at least in some patients with primary myxedema(chronic atrophic autoimmune thyroiditis), antithyroid drug treatment in these patients might be beneficial to disease course. To evaluate the effect of antithyroid drug on the thyrotropin receptor blocking antibody levels, we serially measured thyrotropin-binding inhibitor immunoglobulins(TBII) and thyroid stimulation blocking antibodies(TSBAb) using FRTL-5 cells, antimicrosomal- and antithyroglobulin antibody activities in 7 patients with primary myedema who have blocking TSH receptor antibodies during 6 months of methimazole(MMI, 40mg/day) administration. TBII and TSBAb activities did not change after MMI, but one of them showed stepwise decrease and disappearance of TBII and TSBAb activities. Antimicrosomal- and antithyroglobulin antibody activities decreased significantly after 3 months of MMI administration in those patients. These results suggest a minimal effect of antithyroid drug treatment on the level of thyrotropin receptor blocking antibodies. Persistence of thyrotropin receptor blocking antibodies despite of the decrease in antimicrosomal and antithyroglobulin antibodies might suggest that blocking TSH receptor antibodies of primary myxedema is produced mainly in extrathyroidal tissue in contrast to the thyroid stimulating antibodies of Graves' disease. One patient, whose blocking antibody have disappeared after MMI treatment, is under observation to see if she will remain in remission of hypothyroidism.

- Evaluation of the Usefulness of Free T4 Measured by 2 - Step Iimmunoextraction in the Patients with Thyroid and Non - Thyroid Diseases.
- Bo Youn Cho, Hong Kyu Lee, Jae Hoon Chung, Seok In Lee, Won Bae Kim, Chang Soon Koh
- J Korean Endocr Soc. 1994;10(2):98-104. Published online November 6, 2019
- 1,179 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - Many methods and commercial kits have become available for directly measuring free thyroxine(free T_4). However, most of them are inadequate for routine laboratory use because of their complexity and inaccuracy. Recently, 2-step RIA methods by immunoextraction(2-step immunoextraction) for free T_4 have been developed to improve its accuracy and convenience. We evaluated the usefulness of free T_4 measured by 2-step immunoextraction compared to free T_4 index(FT_4I), free T_4 measured by 1-step RIA, and TSH in 204 patients with thyroid and non-thyroid disease. There were no differences in sensitivities and specificities of free T_4(1-step, 2-step), FT_4I and TSH in the patients with hyperthyroidism and euthyroid nodule. However, the sensitivity of TSH in hypothyroidism was remarkablely higher than the others(100.0% vs. 61.5-81.5%). The sensitivity of free T_4(2-step) was also higher than those of free T_4(1-step), FT_4I and TSH in the patients with non-thyroid disease(94.3% vs. 74.3-83.8%). The values of free T_4 measured by 1-step RIA were significantly lower than those by 2-step immunoextraction, especially in the patients with non-thyroid disease(1.10+-0.04 vs. 1.55+-0.03ng/dL, p<0.05).In conclusion, no significant differences were found in sensitivity and specificity of free T_4(1-step, 2-step), FT_4I, and TSH in the patients with thyroid diseases except in hypothyroidism. However, the sensitivity of free T_4 measured by 2-step immunoextraction was significantly higher than the other tests, especially in the patients with non-thyroid disease. Therefore, free T_4 assay using 2-step immunoextraction is useful to differentiate the non-thyroid disease from thyroid diseases.

- Thyroid
- Prognosis of Differentiated Thyroid Carcinoma with Initial Distant Metastasis: A Multicenter Study in Korea
- Hosu Kim, Hye In Kim, Sun Wook Kim, Jaehoon Jung, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Hee Kyung Kim, Ho-Cheol Kang, Ji Min Han, Yoon Young Cho, Tae Hyuk Kim, Jae Hoon Chung
- Endocrinol Metab. 2018;33(2):287-295. Published online June 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.287
- 5,441 View
- 59 Download
- 31 Web of Science
- 28 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Most patients with differentiated thyroid cancer (DTC) have a favorable prognosis. However, patients with DTC and initial distant metastasis have not been commonly found, and their clinical characteristics have seldom been reported. In this study, we analyzed the clinical features and prognosis of patients with DTC and initial distant metastasis in Korea.
Methods We retrospectively reviewed the clinical data of 242 patients with DTC and initial distant metastasis treated from 1994 to 2013, collected from five tertiary hospitals in Korea.
Results The patients' median age was 51 years, and 65% were women. They were followed for a median of 7 years. Lung was the most common site of distant metastasis: only lung 149 patients (62%), only bone 49 (20%), other single site one (pleura), and combined sites 43 (40 were lung and bone, two were bone and other site, and one was lung and other site). At the time of diagnosis, 50 patients (21%) had non-radioactive iodine (RAI) avidity. Five-year disease-specific survival (DSS) was 85% and 10-year DSS was 68%, which were better than those in previous studies. After multivariate analysis, old age, male sex, metastatic site, and histologic type (follicular type) were significant factors for poor prognosis. However, negative RAI avidity status was not a significant prognostic factor after adjusting for other variables.
Conclusion The prognosis of Korean patients with DTC and initial distant metastasis was better than in previous studies. Old age, male sex, metastasis site, and histologic type were significant prognostic factors.
-
Citations
Citations to this article as recorded by- Case report: A case of hyperthyroidism secondary to bone metastasis of differentiated thyroid cancer
Tingyu Gu, Zhihong Zhao, Yuanyuan Shi, Zhenhua Sun, Yao Wang, Zhiyuan He, Kun Wang
Frontiers in Oncology.2024;[Epub] CrossRef - Theranostics of Thyroid Cancer
Luca Giovanella, Murat Tuncel, Atena Aghaee, Alfredo Campenni, Armando De Virgilio, Petra Petranović Ovčariček
Seminars in Nuclear Medicine.2024;[Epub] CrossRef - Thyroid Hormone Withdrawal versus Recombinant Human TSH as Preparation for I-131 Therapy in Patients with Metastatic Thyroid Cancer: A Systematic Review and Meta-Analysis
Luca Giovanella, Maria Luisa Garo, Alfredo Campenní, Petra Petranović Ovčariček, Rainer Görges
Cancers.2023; 15(9): 2510. CrossRef - Molecular Theranostics in Radioiodine-Refractory Differentiated Thyroid Cancer
Petra Petranović Ovčariček, Alfredo Campenni, Bart de Keizer, Desiree Deandreis, Michael C. Kreissl, Alexis Vrachimis, Murat Tuncel, Luca Giovanella
Cancers.2023; 15(17): 4290. CrossRef - Differentiating pulmonary metastasis from benign lung nodules in thyroid cancer patients using dual-energy CT parameters
Taeho Ha, Wooil Kim, Jaehyung Cha, Young Hen Lee, Hyung Suk Seo, So Young Park, Nan Hee Kim, Sung Ho Hwang, Hwan Seok Yong, Yu-Whan Oh, Eun-Young Kang, Cherry Kim
European Radiology.2022; 32(3): 1902. CrossRef - Feasibility of Recombinant Human TSH as a Preparation for Radioiodine Therapy in Patients with Distant Metastases from Papillary Thyroid Cancer: Comparison of Long-Term Survival Outcomes with Thyroid Hormone Withdrawal
Hsi-Chen Tsai, Kung-Chu Ho, Shih-Hsin Chen, Jing-Ren Tseng, Lan-Yan Yang, Kun-Ju Lin, Ju-Chin Cheng, Miaw-Jene Liou
Diagnostics.2022; 12(1): 221. CrossRef - Long-Term Quality of Life (5-15 Years Post-Thyroidectomy) of Thyroid Carcinoma Patients in Two Tertiary Care Hospitals
Mohammed Yousef Alyousef, Mohammed Khaled Ghandour, Mohammed Al-Mohawes, Mosaad Alnwaisir, Tahera Islam, Khalid Al Qahtani
Cureus.2022;[Epub] CrossRef - Evaluation of Lipocalin-2 and Twist expression in thyroid cancers and its relationship with epithelial mesenchymal transition
Pınar Celepli, İrem Bigat, Sefika Karabulut, Salih Celepli, Sema Hücümenoğlu
Annals of Diagnostic Pathology.2022; 59: 151973. CrossRef - Clinical study of ultrasonic evaluation of T/N staging of differentiated thyroid carcinoma using AJCC 8th staging criteria
Yu Liang, Xingxiang Huang, Zhe Song, Yang Yang, Ju Lei, Mei Ren, Li Tan, Hui Zhang, Francis Moore
PLOS ONE.2022; 17(6): e0269994. CrossRef - Therapeutic challenges in metastatic follicular thyroid cancer occurring in pregnancy: A case report
Claudio Spinelli, Beatrice Sanna, Marco Ghionzoli, Elisabetta Micelli
World Journal of Obstetrics and Gynecology.2022; 11(3): 33. CrossRef - Initial clinical and treatment patterns of advanced differentiated thyroid cancer: ERUDIT study
Juan Antonio Vallejo Casas, Marcel Sambo, Carlos López López, Manuel Durán-Poveda, Julio Rodríguez-Villanueva García, Rita Joana Santos, Marta Llanos, Elena Navarro-González, Javier Aller, Virginia Pubul, Sonsoles Guadalix, Guillermo Crespo, Cintia Gonzál
European Thyroid Journal.2022;[Epub] CrossRef - Male sex is not an independent risk factor for recurrence of differentiated thyroid cancer: a propensity score-matching study
Joonseon Park, Kwangsoon Kim, Dong-Jun Lim, Ja Seong Bae, Jeong Soo Kim
Scientific Reports.2021;[Epub] CrossRef - Evaluation of the 2015 ATA Guidelines in Patients With Distant Metastatic Differentiated Thyroid Cancer
Evert F S van Velsen, Merel T Stegenga, Folkert J van Kemenade, Boen L R Kam, Tessa M van Ginhoven, W Edward Visser, Robin P Peeters
The Journal of Clinical Endocrinology & Metabolism.2020; 105(3): e457. CrossRef - Usefulness of a 3D‐Printed Thyroid Cancer Phantom for Clinician to Patient Communication
Dayeong Hong, Sangwook Lee, Taehun Kim, Jung Hwan Baek, Won Woong Kim, Ki‐Wook Chung, Namkug Kim, Tae‐Yon Sung
World Journal of Surgery.2020; 44(3): 788. CrossRef - Estimating the Growth Rate of Lung Metastases in Differentiated Thyroid Carcinoma: Response Evaluation Criteria in Solid Tumors or Doubling Time?
Eyun Song, Jonghwa Ahn, Min Ji Jeon, Sang Min Lee, Jeong Hyun Lee, Tae Yong Kim, Jung Hwan Baek, Won Bae Kim, Young Kee Shong, Won Gu Kim
Thyroid.2020; 30(3): 418. CrossRef - Personalized management of differentiated thyroid cancer in real life – practical guidance from a multidisciplinary panel of experts
Alfredo Campennì, Daniele Barbaro, Marco Guzzo, Francesca Capoccetti, Luca Giovanella
Endocrine.2020; 70(2): 280. CrossRef - Unusual metastases from differentiated thyroid cancers: A multicenter study in Korea
Jee Hee Yoon, Min Ji Jeon, Mijin Kim, A. Ram Hong, Hee Kyung Kim, Dong Yeob Shin, Bo Hyun Kim, Won Bae Kim, Young Kee Shong, Ho-Cheol Kang, Domenico Albano
PLOS ONE.2020; 15(8): e0238207. CrossRef - Extended Real-World Observation of Patients Treated with Sorafenib for Radioactive Iodine-Refractory Differentiated Thyroid Carcinoma and Impact of Lenvatinib Salvage Treatment: A Korean Multicenter Study
Hye-Seon Oh, Dong Yeob Shin, Mijin Kim, So Young Park, Tae Hyuk Kim, Bo Hyun Kim, Eui Young Kim, Won Bae Kim, Jae Hoon Chung, Young Kee Shong, Dong Jun Lim, Won Gu Kim
Thyroid.2019; 29(12): 1804. CrossRef - Clinical outcomes and prognostic factors in patients with no less than three distant organ system metastases from differentiated thyroid carcinoma
Xin-Yun Zhang, Jian-Wen Sun, Zhong-Ling Qiu, Yang Wang, Xiao-Yue Chen, Jin-Hua Zhao, Quan-Yong Luo
Endocrine.2019; 66(2): 254. CrossRef - Molecular Profile and Clinical Outcomes in Differentiated Thyroid Cancer Patients Presenting with Bone Metastasis
Nilma Malik, Alyaksandr V. Nikitski, Elie Klam, Jason Hunt, Benjamin Witt, Barbara Chadwick, Yuri E. Nikiforov, Devaprabu Abraham
Endocrine Practice.2019; 25(12): 1255. CrossRef - Improved survival after early detection of asymptomatic distant metastasis in patients with thyroid cancer
Hosu Kim, So Young Park, Jaehoon Jung, Jung-Han Kim, Soo Yeon Hahn, Jung Hee Shin, Young Lyun Oh, Man Ki Chung, Hye In Kim, Sun Wook Kim, Jae Hoon Chung, Tae Hyuk Kim
Scientific Reports.2019;[Epub] CrossRef - Unusual metastases from differentiated thyroid carcinoma: analysis of 36 cases
Anabela Zunino, Fabián Pitoia, Eduardo Faure, Adriana Reyes, Mónica Sala, Rosana Sklate, Verónica Ilera, Inés Califano
Endocrine.2019; 65(3): 630. CrossRef - The Prognosis of Papillary Thyroid Cancer with Initial Distant Metastasis is Strongly Associated with Extensive Extrathyroidal Extension: A Retrospective Cohort Study
Young Ki Lee, Daham Kim, Dong Yeob Shin, Cho Rok Lee, Eun Jig Lee, Sang-Wook Kang, Jandee Lee, Jong Ju Jeong, Kee-Hyun Nam, Woong Youn Chung, Cheong Soo Park
Annals of Surgical Oncology.2019; 26(7): 2200. CrossRef - Risk Factors for Distant Metastasis in Follicular Thyroid Carcinoma in Korea
Shin Dol Jo, Joon-Hyop Lee, Suk Ha Kang, Yun Yeong Kim, Yong Soon Chun, Heung Kyu Park, Sang Tae Choi, Jin Mo Kang, Yoo Seung Chung
Journal of Endocrine Surgery.2019; 19(1): 1. CrossRef - Expression levels of ARHI and Beclin1 in thyroid cancer and their relationship with clinical pathology and prognosis
Houwei Zhu, Yanqing Qu
Oncology Letters.2019;[Epub] CrossRef - 甲状腺腫瘍治療の最新情報
Nippon Jibiinkoka Gakkai Kaiho.2018; 121(11): 1336. CrossRef - Clinical Outcomes of Differentiated Thyroid Cancer Patients with Local Recurrence or Distant Metastasis Detected in Old Age
Ji Min Han, Ji Cheol Bae, Hye In Kim, Sam Kwon, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2018; 33(4): 459. CrossRef - Efficacy and Affecting Factors of 131I Thyroid Remnant Ablation After Surgical Treatment of Differentiated Thyroid Carcinoma
Chen Wang, Hongcui Diao, Ping Ren, Xufu Wang, Yangang Wang, Wenjuan Zhao
Frontiers in Oncology.2018;[Epub] CrossRef
- Case report: A case of hyperthyroidism secondary to bone metastasis of differentiated thyroid cancer


 KES
KES

 First
First Prev
Prev



